2 Jul 2018
Investigation of dry FIP in a domestic shorthair kitten
Sarah Tayler discusses Rosie, a four-month-old domestic shorthair with a two-month history of diarrhoea, and how she underwent diagnosis.

Image: Kirill Vorobyev / Adobe Stock.
Rosie is a four-month-old domestic shorthair that presented with a two-month history of diarrhoea, unresponsive to diet change or fenbendazole therapy, and having had a seizure-like episode on the day of presentation.
Rosie has had diarrhoea for two months, but has always been normal in every other aspect. She has had various changes to her diet and two five-day courses of fenbendazole therapy, with little to no effect. The evening of presentation she had an episode where she was sat with the owner, then went vacant, staggered and collapsed on to her side and went rigid. She urinated and defecated during the episode.
On presentation, Rosie is bright, but small for her age, weighing 1.35kg. Her heart rate is 240bpm and her mucous membranes are pale. Her respiratory rate is 60 breaths/minute and her rectal temperature is 39.5°C. Neurological examination is unremarkable.
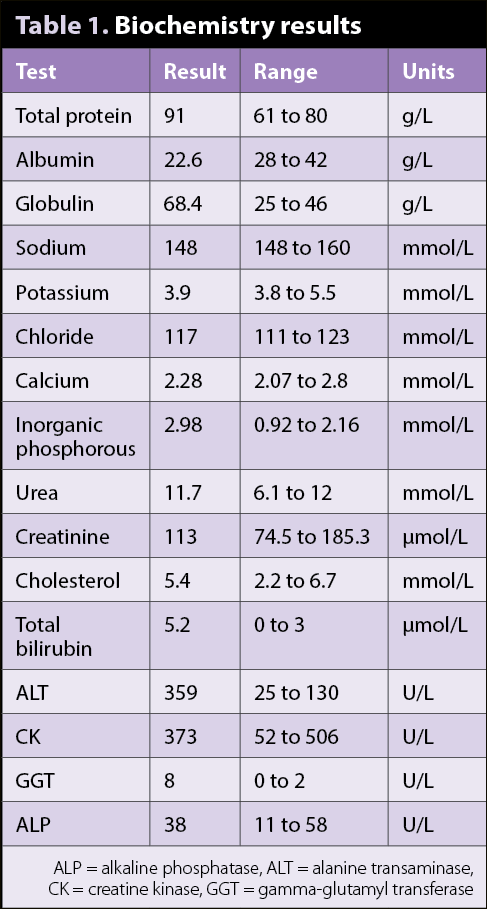
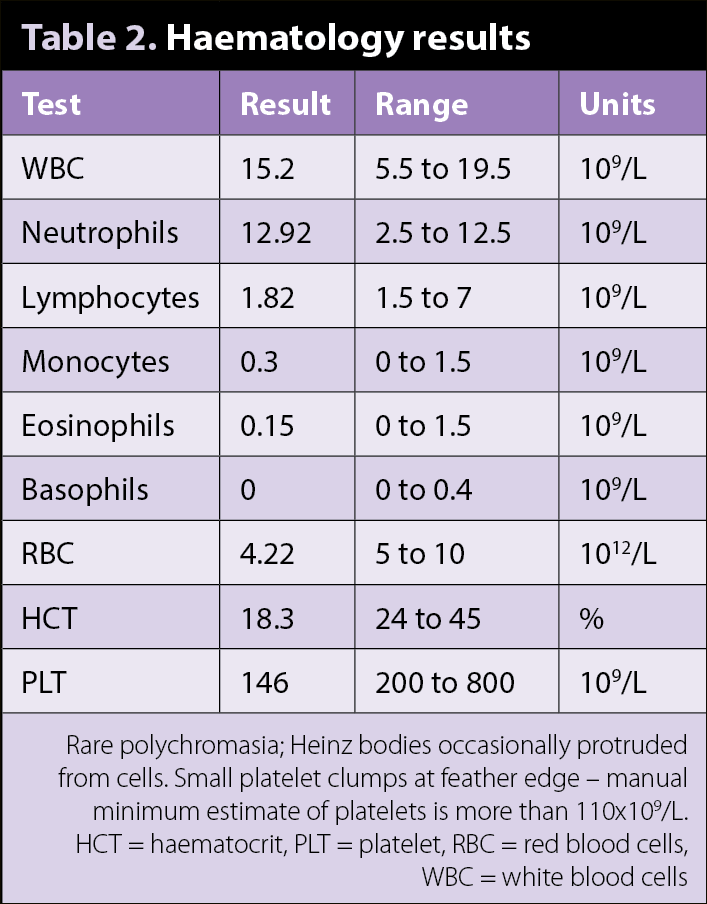
Emergency blood work performed on admission to the hospital reveals a PCV of 15% and total proteins of 107g/L, measured by refractometer. Haematology, including blood smear examination, and biochemistry reveal moderate hyperglobulinaemia, mild hypoalbuminaemia, mildly increased total bilirubin, increased alanine transaminase, increased gamma-glutamyl transferase activities and a moderate non-regenerative anaemia (Tables 1 and 2). Patient-side ultrasound of the abdomen and thorax reveals no pleural or peritoneal effusion.
Question
You suspect dry FIP based on the presentation and initial blood results. What tests can you use to support this diagnosis?
Answer
FIP presents a diagnostic dilemma, as the only confirmatory test is postmortem examination. Routine blood work in Rosie’s case raised the clinical suspicion for FIP, but, due to the associated grave prognosis, further tests were recommended to ensure the owner could be counselled on how to manage Rosie with the highest level of confidence possible.
The most commonly encountered changes on routine bloodwork are lymphopenia, mild non-regenerative anaemia, hypergammaglobulinaemia, hypoalbuminaemia, hyperbilirubinaemia and biochemical changes related to affected organs, such as raised liver enzymes activities and azotaemia. Albumin:globulin ratios below 0.8 may raise the suspicion of FIP and, in this case, was 0.33.
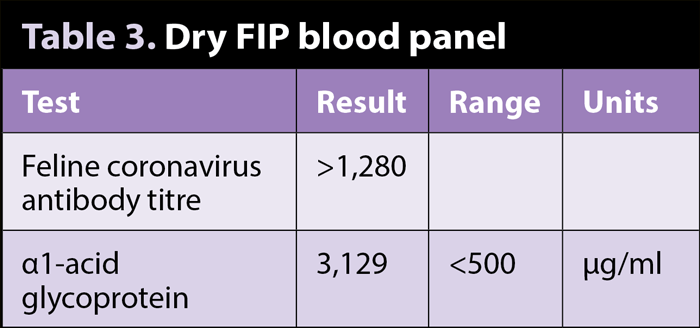
Feline coronavirus antibodies and α1-acid glycoprotein (Table 3) were run on blood and both moderately increased. The coronavirus antibody titre is unable to differentiate between cases that have been exposed to feline coronavirus and those that have undergone in vitro mutation to FIP virus. Alpha-1-acid glycoprotein is an acute phase protein produced by the liver and can be elevated in any inflammatory condition. Therefore, both results must be interpreted carefully considering the individual animal.
Abdominal ultrasound was performed, which revealed a bilateral nephropathy and a diffuse splenopathy. Fine needle aspirates (FNAs) of the liver, spleen and kidneys were performed to look for macrophagic inflammation that may be suitable for immunohistochemistry to detect coronavirus in macrophages. This test carries a relatively high level of sensitivity and specificity, but relies on the presence of significant numbers of macrophages in the sample. This is of greater use in the effusive form of FIP, where fluid is readily available and easily obtained for analysis.
However, in Rosie’s case, the FNAs were unremarkable; therefore, we were unable to run these direct tests. Biopsies can be taken of affected organs by laparoscopy or laparotomy for immuno-histochemistry; however, due to the invasive nature of the procedure, is rarely undertaken.
MRI and CSF analysis can also be of use in cases of dry FIP with neurological signs. CSF analysis may reveal an elevated protein and pleocytosis consisting mainly of neutrophils, macrophages and lymphocytes. Reverse transcriptase PCR can be performed on CSF, with one study showing a specificity of 100% and a sensitivity of 85.7% if used only on cases with neurological/ocular signs. These were not performed in Rosie’s case due to the high level of clinical suspicion and more invasive nature of these tests.
In conclusion, dry FIP presents a diagnostic dilemma due to the relative difficulty in obtaining samples suitable for direct detection of virus and the inability of diagnostic tests to differentiate between pathogenic and non-pathogenic virus. Taking Rosie’s entire clinical picture into account, dry FIP was thought to be very likely, and this was supported by the axillary diagnostic tests carried out.
Unfortunately, she progressed quickly to develop respiratory distress and ocular lesions and, therefore, was euthanised four days after presentation.
Latest news