1 Apr 2019
Applying use of 3D printing for appendicular surgery
Kevin Parsons investigates how 3D printing can aid in surgery, focusing on the manufacture of custom implants and prosthetics.

A shoulder joint used as a visual reference in surgery, and a limb model to rehearse surgery. Image: CBM Medical.
The use of 3D printing technology is rapidly evolving, and having a significant impact in human and veterinary medicine and surgery.

It is difficult to predict where this will lead; however, with an ever-increasing array of materials that can be printed – including biocompatible plastics, titanium, titanium alloys and biological materials – patient-specific implants and surgical guides are no longer a thing of the future and readily available for use in the veterinary orthopaedic surgical field.
Four main areas are applicable to orthopaedic practice where 3D technologies are being used, namely:
1. The production of bone models to assist with surgical planning.
2. The creation of drilling, cutting and/or repositioning guides that can be used in applications such as the treatment of angular limb deformities or fracture reduction.
3. The manufacture of customised patient-specific implants.
4. Patient-specific prostheses.
Anatomical bone models
CT and MRI digital imaging and communications in medicine (DICOM) data can be used to print 3D models. A range of printable materials are available depending on the model’s intended use.
Models can be used for educational purposes (such as for demonstrating planned procedures to students, residents and owners), improving the understanding of a complex problem (such as in angular limb deformities), pre-contouring of plates, the construction of complex circular or hybrid fixators prior to surgery, and planning/rehearsing surgery.
The ability to plan has several benefits, including improved surgical accuracy, reduced surgical time, and improved bone reduction and alignment. In many situations, the time-saving benefits more than compensate for the extra costs incurred from model manufacture. Models can be created out of a range of materials. Recently, the author has been using autoclavable polymers to allow the models to be handled and used patient side on the operating room.
Surgical guides
Polymer and metal cutting, drilling and repositioning surgical guides can be produced using DICOM data imported into computer-aided design (CAD) software.
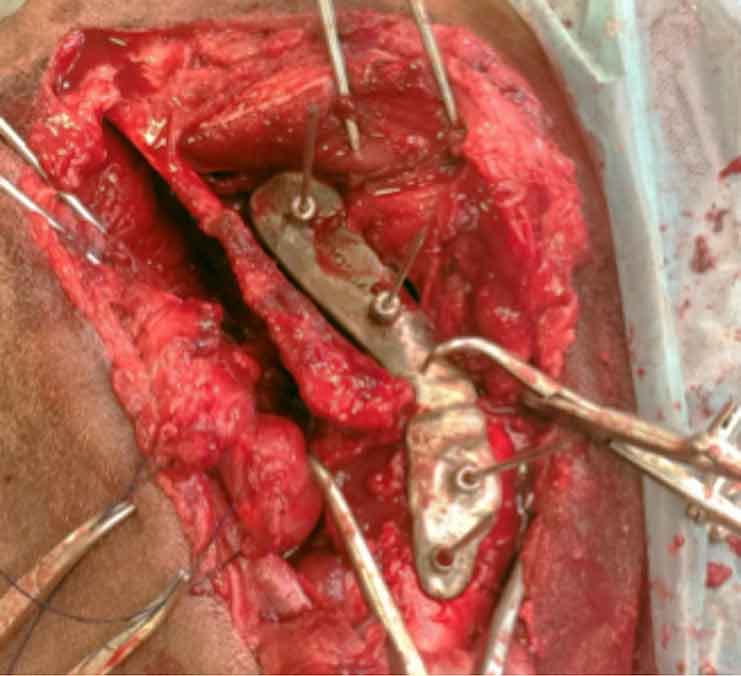
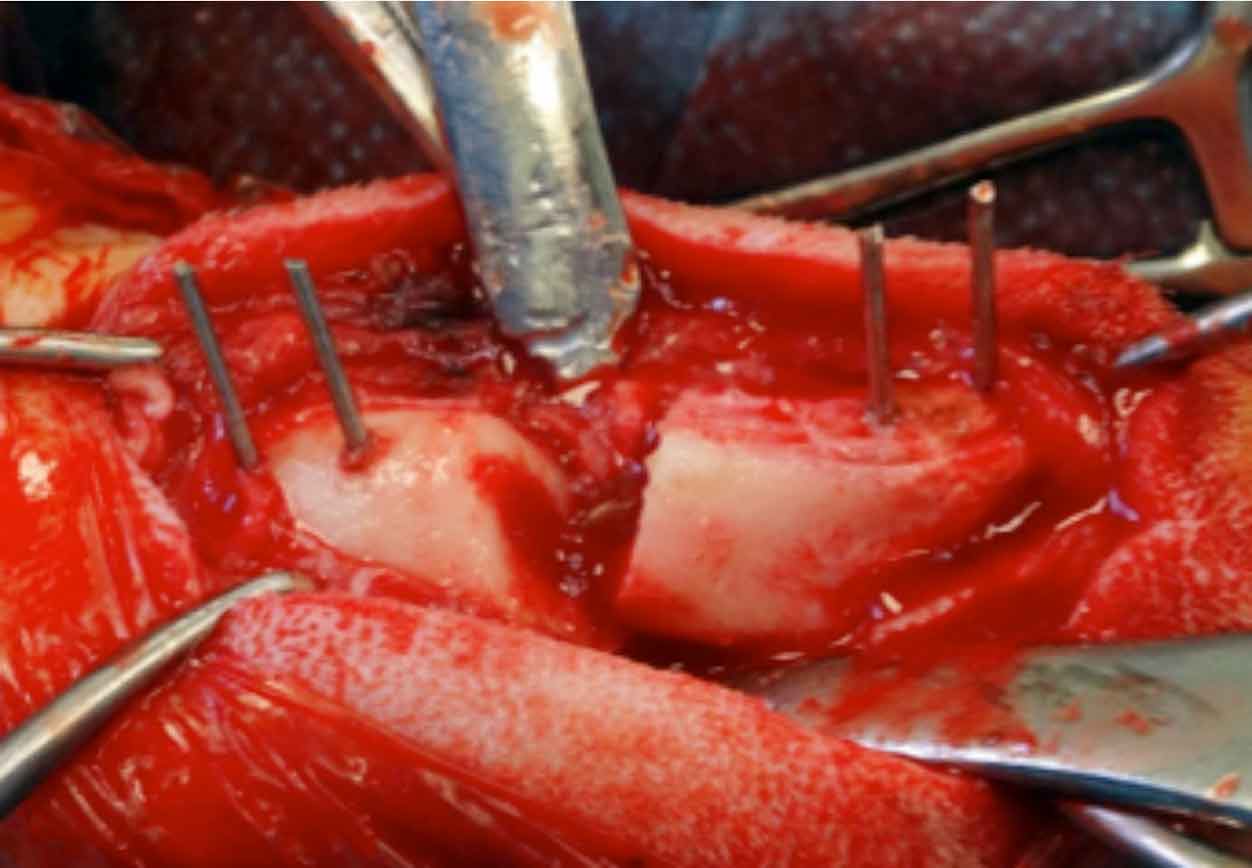
These guides can be created to assist in a wide range of surgical procedures, including angular limb deformity correction, shoulder arthrodesis surgery (or any other arthrodesis surgery), fracture reduction, medial patellar luxation femoral osteotomy surgery and drill guides for spinal surgery.

These guides are used to translate surgical plans precisely and predictably into the operating theatre. It is important to remember although guides can improve predictability and accuracy of surgery, basic surgical principles must continue to be followed. Soft tissues must be respected.
Surgical implants
Technology is readily available to print customised implants. This is an exciting development. Custom implants match exactly to the individual patient anatomy/problem can be created using CAD software.
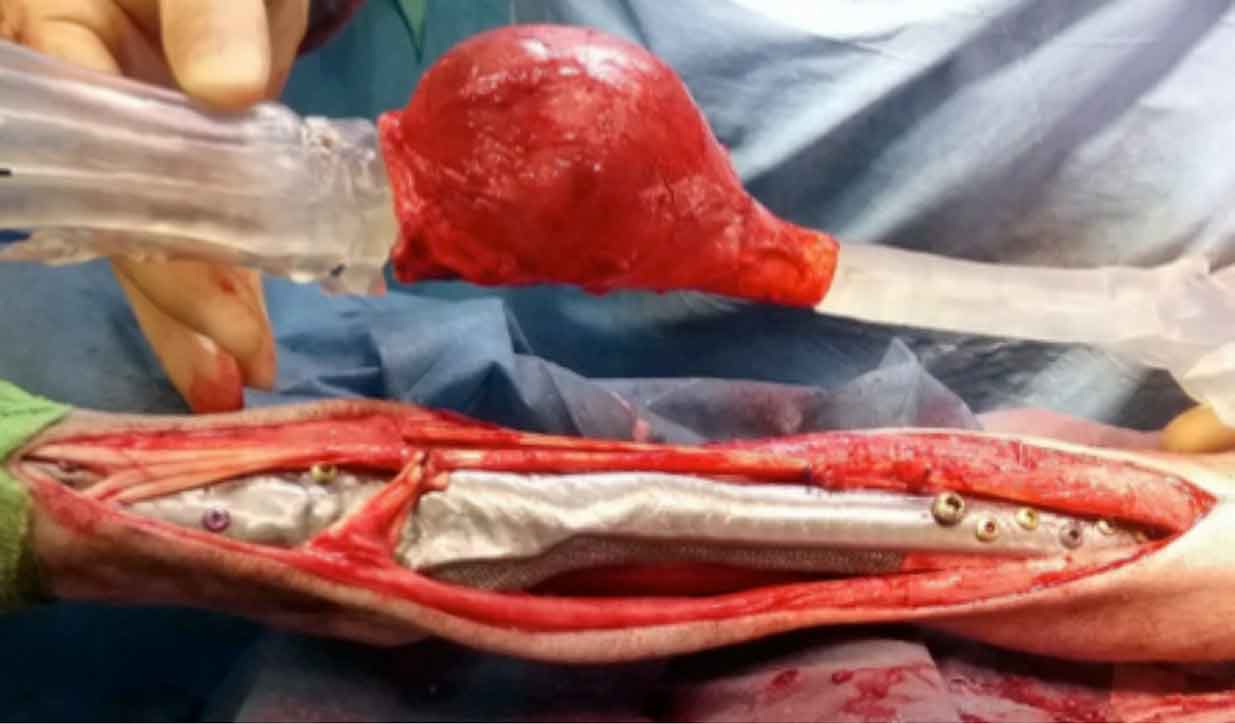
Implants consisting of a perfectly contoured plate combined with bone bridging scaffold can be created and are particularly useful in load-bearing areas (such as during tumour excision limb sparing surgery).
Custom innovations
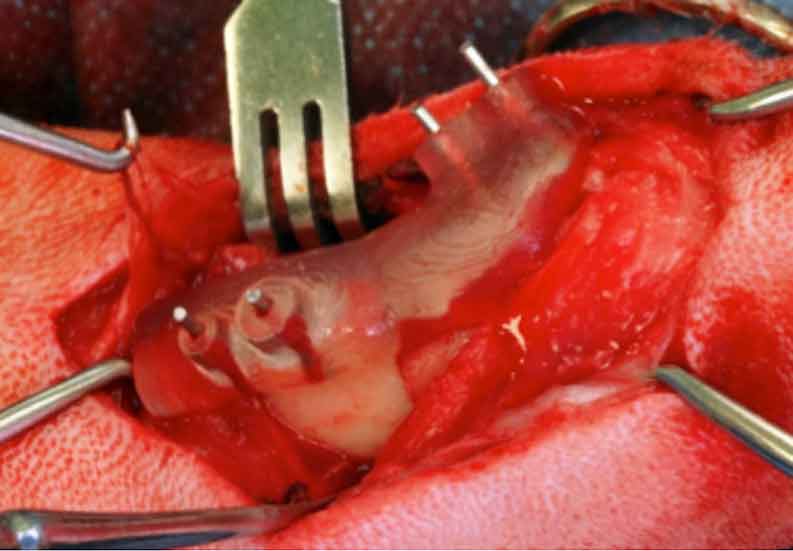
Medical innovations, such as customised prosthesis, can be designed based on an individual patient’s anatomy.
Applying 3D printing technology in veterinary orthopaedics
Angular limb deformities
Antebrachial angular limb deformities are commonly seen in chondrodysplastic dogs, such as shih-tzus and bassets, and are caused by asynchronous growth of the paired bones of the forelimb. Traumatic injuries at a young age can also present similarly in any breed.
The aims of treatment for any angular limb deformity are to alleviate pain (most commonly by addressing joint incongruity), correct the bony deformity and address clinically significant limb shortening. Further growth potential also needs to be factored into planning.
Each case should be considered independently, and the timing of surgery and the surgical methods employed carefully considered to optimise outcome. The challenge is increased by the fact that for limbs of chondrodystrophic dogs, contralateral limbs are often affected to varying degrees and a lack of published breed-specific normal values exists.
Where appropriate surgery usually involves one, or a combination of, an ulna ostectomy or osteotomy (when joint incongruity or pain is present) and a radial osteotomy and ulna ostectomy/ostectomy if there is a moderate to severe radial valgus, varus, rotation or pro/recurvatum. Planning of this radial osteotomy can be challenging.
It is well described that the determination of the centre of rotation of angulation (CORA) is important to identify where to centre osteotomies. Deformities are characterised as uniapical and biapical, dependent on whether one or two CORAs exist.
In addition to determining frontal and sagittal plane components of deformities, torsion must be considered. Research has demonstrated that torsion interferes with accurate radiographic measurement of frontal plane deformities. This makes radiographic interpretation and calculations for correction challenging and fraught with miscalculation.
Once a full assessment has been made, one needs to decide whether to perform an acute correction or a gradual correction (most commonly using a circular external fixator).
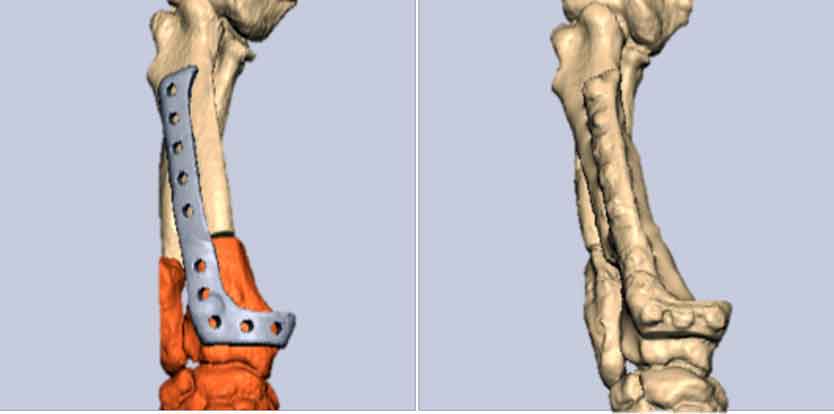
CT allows full characterisation of the deformity. The subsequent creation of 3D anatomical models allows a rehearsal surgery that contributes to successful planning and execution of the surgical correction.
Until recently, the author primarily used external skeletal fixators for these cases. This process is greatly assisted by the creation of 3D anatomic bone models to allow surgical rehearsal. Use of virtual 3D surgical planning has become accessible. Working with CAD software, imaging data is processed to create on-screen 3D models. This allows ”virtual” surgery to be performed, with the creation of osteotomies and realignment of bone segments.
Once completed on the virtual screen, cutting and repositioning guides can be created. These guides allow precise correction of the deformity during surgery with predictable bone realignment to match that of the virtual surgery performed previously.
Although improving the predictability of limb realignment, many factors are still considered in these complex cases. Firstly, many deformities are biapical. Despite this, it seems the majority can be addressed with a single radial and ulna osteotomies.
When performing acute corrections with internal fixation, the ability to make postoperative adjustments is limited. It is, therefore, important to fully assess whether carpal laxity exists. Significant stretching of the joint capsule and collateral ligaments on the convex side of a deformation can be observed and, in these cases, addressing the bony deformity alone may not be enough to resolve the problem.
Owners need to be aware of this in advance, as it is disappointing where laxity persists following surgery as this can negatively affect the long-term function and may necessitate further surgery. The effect of addressing bony deformities on the surrounding soft tissues also needs to be considered. In some cases of marked pro-curvatum, the caudal soft tissues may not tolerate acute lengthening.
Limb sparing
Following appropriate staging and case consideration the options available for managing the pain associated with appendicular osteosarcoma include amputation, radiotherapy and limb-sparing surgery.

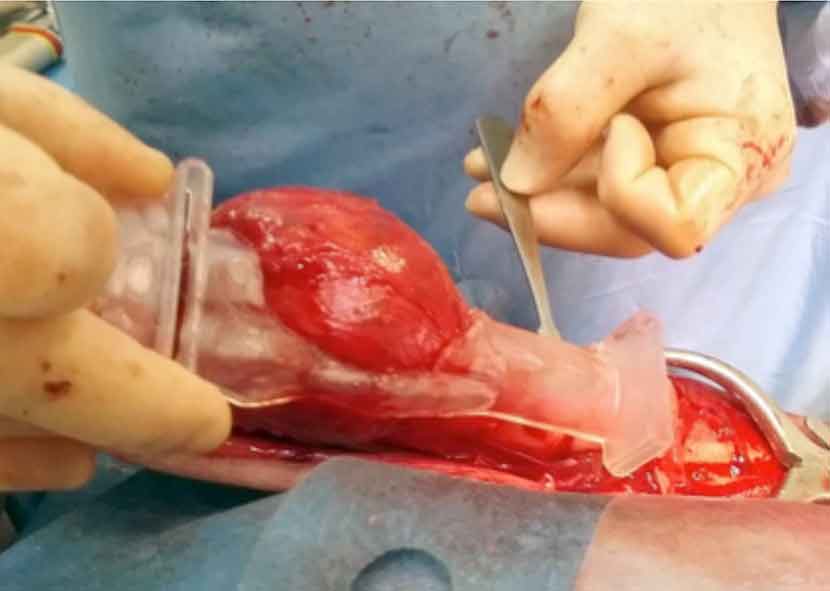
3D printing techniques can be used to fabricate cutting guides for more precise resection of the tumour within bone. This can be followed by the implantation of customised implants, which include a metal spacer attached to the remaining bone. In addition to improving accuracy, this technique allows significantly shorter surgical time.
This surgery can be a good option for large and giant breed dogs where amputation may not be well tolerated.
Limb prosthesis
Customised patient-specific socket prosthesis can be manufactured for a range of patients following amputation or around the birth abnormality. This may prove to be a successful option in patients that are poor candidates for limb amputation alone or where severe limb deformities exist.
Acknowledgements
The author would like to thank CBM Medical (Swansea) for the images and collaboration with cases included in this report. Neil Burton (Wear Referrals, Bradbury) and Jonathon Deacon (Moorview Vets, Cramlington) are acknowledged for the intraoperative shoulder arthrodesis and limb sparing images.