23 Nov 2015
An update to lymphoma in dogs

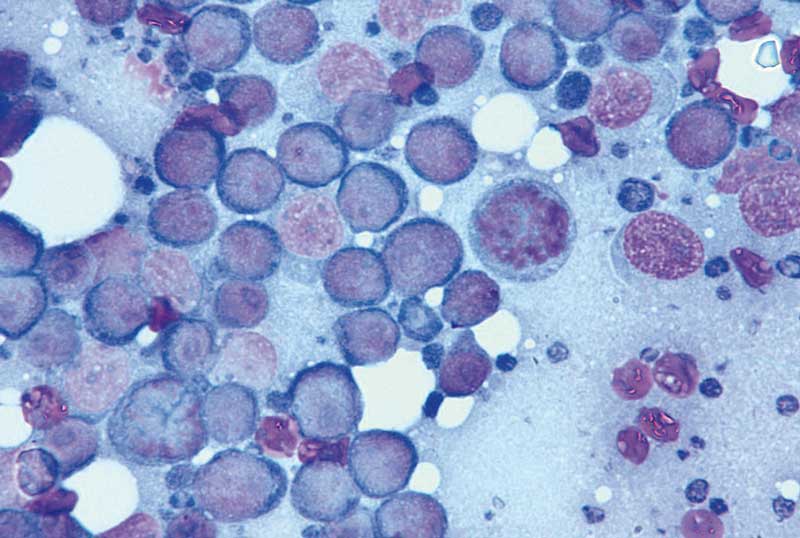
Figure 1. Lymphoma cytology. Lymph node fine-needle aspirate of a dog with typically high-grade/large cell lymphoma.
Lymphoma is a neoplasm arising from the malignant transformation of lymphocytes. Generally, this is a disease of middle-aged to older dogs, although many young dogs can develop the condition.
Various breeds are said to be predisposed to this neoplasm including the boxer, Labrador, golden retriever and bullmastiff; however, any breed or cross-breed dog can develop the disease. The vast majority of dogs develop multicentric lymphoma, where the dog presents either clinically well, or with non-specific signs of disease, with generalised, firm enlargement of all multiple peripheral lymph nodes.
Pathology
The majority of dogs have a type of lymphoma analogous to non-Hodgkin lymphoma in humans based on histology. Most cases of the disease in the dog are high-grade lymphoma, where, histologically, the lymphocytes are immature, large “blast” cells and the disease develops quickly and, without appropriate therapy, rapidly results in clinical decline of the patient. Occasionally, some dogs have a low-grade or lymphocytic/small cell lymphoma consisting of small lymphocytes that often appear cytologically/histologically very similar to normal, small lymphocytes.
Subtyping lymphoma (for example, immunoblastic, centroblastic, Burkitt’s, or marginal zone lymphoma) in the veterinary field is under way, but not reported by most UK pathologists and is not in routine clinical use. However, practitioners can request immunophenotyping (B-cell or T-cell lymphoma), which does have strong prognostic significance and may affect therapeutic decisions (see later).
Clinical signs and differentials
Most dogs present with generalised, markedly enlarged and non-painful peripheral lymphoma nodes; however, some dogs can present a diagnostic challenge due to internal disease (nodes, visceral organs). For the dog that presents with significant, generalised lymph node enlargement there are realistically rather few other differentials in the UK.
Pyoderma/generalised skin disease is a major problem that needs to be ruled out as this can cause generalised lymphadenopathy and also hamper cytological interpretation because reactive nodes contain a higher number of immature cells. Biopsy may be required in these cases. Other infectious agents that need to be ruled out, such as tick-borne disease and fungal disease, are extremely rare in the UK, particularly with no foreign travel history. Immune-mediated diseases can also cause lymphadenopathy, but usually one would see supporting evidence for these on haematology, biochemistry and urinalysis, and cytology would hopefully distinguish from lymphoma.
Diagnosis
A diagnosis of lymphoma in the dog is commonly achieved with cytology of a fine-needle aspiration (FNA) or histology of a biopsy specimen.
As dogs usually have easily accessible peripheral nodes that are often very large and most commonly have high-grade disease, the diagnosis can be made by FNA alone in the vast majority of cases – that is more than 90% (Figure 1). This can be performed without sedation in most patients.
The submandibular nodes should be avoided if possible (they drain the oral cavity and can be more reactive, and specimens more difficult to interpret). Biopsy/nodectomy of the prescapular nodes seems to be associated with a higher risk of seroma and so the popliteal nodes should be biopsied if appropriate. Obviously, the nodes most clearly diseased should be sampled regardless of their location.
Immunohistochemistry and flow cytometry
Occasionally, the pathologist is unable to tell if a population of lymphocytes in a biopsy specimen is neoplastic. In this situation immunohistochemistry (IHC) may be recommended to try to distinguish whether the cells exhibit the same surface markers (that is, in neoplasia the cells should be all B-cells or all T-cells). Cytology slides, even when already stained, can be sent for the PCR for antigen receptor rearrangements (PARR) clonality test, which works on the principle that if the cells are neoplastic they should originate from a single clone. Therefore, if this test is positive, it is highly specific for neoplasia – that is lymphoma.
Flow cytometry can be performed on lymph node aspirates (FNA is performed in the normal way, but the material from aspirates is squirted into a special fluid rather than on to a slide to keep the cells in liquid suspension). A flow cytometer then separates the cells based on size, complexity and cell surface markers and can be very useful for diagnosis and immunophenotyping of lymphomas.
Some flow markers applied to lymphoma cells can also provide prognostic information (that is major histocompatibility complex class two-plus lymphomas have a better prognosis). These more sophisticated tests, in addition to classical histology/cytology, are particularly useful for the cases of low-grade lymphoma where diagnosis based on cellular morphology alone is often impossible.
Is it worth knowing if it is B-cell or T-cell lymphoma?
Immunophenotyping is commonly performed (immunohistochemistry on biopsy samples, PARR, flow cytometry) to show whether neoplastic lymphocytes are cluster of differentiation (CD) 3-positive (T-cell) or CD21/CD79a-positive (B-cell). This information is highly prognostic, with T-cell lymphomas typically exhibiting poorer response to chemotherapy, less durable responses and poorer overall survivals. However, lymphoma is a very heterogeneous disease and there are dogs with T-cell lymphoma that do extremely well and dogs with B-cell lymphoma that respond very poorly to therapy.
Some evidence shows treating T-cell lymphomas with different protocols to the conventional cyclophosphamide, doxorubicin, vincristine and prednisolone (CHOP) protocols (that is lomustine, vincristine, procarbazine and prednisolone [LOPP]; mechlorethamine, vincristine, procarbazine and prednisolone [MOPP]; or lomustine-inclusive CHOP protocols) may result in a better outcome. Indeed, some oncologists routinely use these protocols as a first-line therapy for dogs with T-cell lymphomas and the author’s recommendation is to perform immunophenotyping in all cases, with a view to offering owners a variety of protocols specific to the individual’s disease.
Staging

Staging of all cancer patients is appropriate, recommended and can yield important information. For a dog with lymphoma, this would typically involve a dorsoventral and lateral thoracic radiograph and an abdominal ultrasound (Figure 2). However, particularly in the case of the clinically well dog with generalised lymphadenopathy, lymphoma is one of the few tumours where staging may be omitted after discussion with the owner, particularly if there are financial concerns. This is because the treatment will probably not be changed by the results of staging. Lymphoma, in the vast majority of canine patients, is a systemic disease with polysystemic involvement, and so conventional systemic chemotherapy is the only appropriate therapy.
Bone marrow aspirate to document marrow infiltration (and thus stage five disease) is performed by some. This can yield significant prognostic information (dogs with stage five lymphoma do significantly worse); however, this does not generally change the treatment recommendations and so can be excluded from the routine staging procedure in the majority of cases, unless the owner wishes for as much prognostic data as possible. Again, there are many dogs with stage five disease that do extremely well with treatment.
The author would advise any dog with significant cytopenias be considered for bone marrow aspiration as this may indicate leukaemia as opposed to lymphoma, which has a profoundly different prognosis.
In any case of apparently localised lymphoma (for example, nasal, solitary skin mass, rectal mass), staging becomes much more important, as if only local treatment is planned (such as surgery or radiation therapy) one must be sure there is no systemic involvement. Even in this scenario, systemic disease may appear days, weeks or months later and the owner must be aware of this. For this reason, many oncologists recommend adjuvant systemic chemotherapy in these cases in addition to the local treatment at the time of diagnosis, while others hold off until signs of systemic progression ensue. There are arguments for both approaches and the debate is still to be settled.
Treatment
As the majority of canine cases are multicentric in nature, systemic chemotherapy is the only appropriate therapy for these dogs. Several protocols have been studied and the main ones will be briefly discussed.
Madison-Wisconsin 25-week protocol
The Madison-Wisconsin 25-week discontinuous protocol consists of using the drugs L-asparaginase, vincristine, cyclophosphamide, doxorubicin/epirubicin and prednisolone – that is, a CHOP-based protocol. This protocol, originally reported by Garrett et al (2002) led to a 94% complete response rate, with 100% of those patients achieving a second remission after re-induction with the same protocol at relapse.
This protocol has no maintenance phase and if the animal is in remission at 25 weeks, treatment is withdrawn and reinstituted when relapse occurs. This may lead to greater responsiveness after loss of remission by lack of selection for resistance during the second rapid growth phase. It is generally well accepted protocols without extended maintenance phases are as efficacious as those with protracted maintenance phases. Median survival is around 12 months with this protocol. It is also well accepted dogs benefit from the addition of doxorubicin/epirubicin to their chemotherapy treatment.
Some studies have questioned the benefit of adding L-asparaginase to this protocol and, therefore, some oncologists prefer to “save” this drug for use at relapse. Some oncologists modify this protocol by substituting the cyclophosphamide for lomustine in cases of T-cell lymphoma – making it a 27-week protocol.
High-dose COP
High-dose COP consists of using only vincristine, cyclophosphamide and prednisolone. This is a less expensive and less time-consuming protocol; however, understandably, this results in a lower percentage of patients achieving remission and for shorter survivals. Generally, 70% to 75% of patients can be expected to attain a remission for around seven-and-a-half months.
Some dogs can do extremely well on COP with protracted remission and survival times. Some also believe doxorubicin can be instituted as a “rescue” once COP has ceased to be effective and thus result in similar remission/survival characteristics to using Madison-Wisconsin from the outset. However, oncological principles would suggest it would be most effective to use all the drugs together from the outset and, if possible, this should be performed. The author always advises clients to follow a CHOP-based protocol if financially/logistically possible.
Single agent doxorubicin or epirubicin
Single agent doxorubicin or epirubicin consists of five to six treatments with doxorubicin (30mg/m2 or 1mg/kg if less than 15kg) as a single agent given once every three weeks. The advantages are reduced visits, a reduced number of treatments and ease of only having to worry about one drug and its associated side effects. This is effective in around 59% to 79% of patients, with median survivals of around seven to nine months.
These drugs can cause cardiotoxicity. In the acute sense this can manifest as arrhythmias and it is recommended the drug be given slowly rather than as a bolus for around 20 minutes. ECG monitoring can be used if there is any concern during the infusion and pulse characteristics and auscultation can be intermittently performed during infusion.
Chronically, poor systolic dysfunction can become apparent, mimicking dilated cardiomyopathy, and this is related to the total cumulative dose, which is generally seen more commonly with doses of more than 200mg/m2, but can be seen at lower doses. For this reason, it is advisable to attain a baseline echocardiogram prior to therapy, particularly in “at risk” breeds. While this toxicity should not be ignored, the incidence of cardiac toxicity is extremely low and if an echocardiogram cannot be performed for financial or logistical reasons, in the absence of significant cardiac signs, the author would not withhold treatment. Interestingly, this toxicity has not been documented in the cat, where nephrotoxicity is more of a problem.
Epirubicin may cause less cardiac toxicity compared with doxorubicin and appears to have just as good an effect in canine lymphoma.
These drugs are severe vesicants and a long, well-placed and well-secured intravenous catheter must always be placed and someone must monitor the infusion constantly. It can result in tissue sloughing requiring extensive surgery/amputation if extravasation occurs. If this occurs, treatment can be attempted with the iron-chelating dexrazoxane and details can be obtained from a clinical oncologist.
Rescue protocols
Only a very small proportion of dogs will be “cured” with chemotherapy and never experience tumour relapse. Most dogs relapse eventually. If the dog has finished a discontinuous protocol, this should be reinstituted and continued if effective. If this is no longer effective, or if the dog relapses while still receiving the protocol for the first time, treatment needs to be changed.
Once the original drugs have ceased to be effective, “rescue” agents can be used to good effect; however, the tumour is usually relatively drug-resistant by this point and remission times are substantially shorter than at diagnosis. Depending on the protocol, around 30% to 50% of patients achieve a partial or complete remission with these protocols from between some weeks to a short number of months.
Occasionally, a dog will have a really pleasing and durable response to these rescue agents. The author generally finds multi-agent protocols, such as dexamethasone, melphalan, actinomycin D and cytarabine (DMAC) most effective and well-tolerated, but some dogs have very good responses to single agent lomustine (CCNU) and other various drugs.
Owners need to be aware once rescue is considered/instituted, the prognosis is guarded and they need to be prepared that the tumour is becoming difficult to control.
Individual protocols
A variety of drugs/doses and combinations can be formulated for individuals with particular needs – whether it be financial, owner logistical issues or temperament-related. Consultation with a clinical oncologist is recommended for such cases.
Breed differences
Breeds predisposed to ivermectin toxicity, for example, collie-type breeds, can also be very sensitive to certain chemotherapy agents such as vincristine and the anthracyclines. This is because they have a mutation in the gene ABCB1, which encodes p-glycoprotein, a cellular efflux pump. Defects thus disable the efflux of substances such as chemotherapy agents from cells and result in increased toxicity. This can manifest as haematological or gastrointestinal toxicity. Blood can be sent to test for the mutation in susceptible breeds and, while results are pending, the protocol can be altered so therapy is started with a drug class not dependent on p-glycoprotein mechanisms, such as alkylating agents (for example, cyclophosphamide).
Drugs such as vincristine can still be given to these patients; however, they usually require to be given at lower doses to prevent myelosuppression and gastrointestinal toxicity. For example, a dose of 0.5mg/m2 can be tried as opposed to 0.7mg/m2 of vincristine for the first administration. Some dogs need even lower doses than this that would normally be seen as sub-therapeutic in “normal” dogs.
Prognosis
Generally, the outlook for the typical dog with multicentric, high-grade lymphoma is around a year. Some dogs can do significantly better than this; alternatively, some can do significantly worse and often this can be predicted from the presence of one or more negative prognostic factors. Without therapy many of these dogs will succumb within one or two months.
Dogs with the rarer low-grade disease can actually have a much better outlook. They often present with mild to moderate, slowly progressive, regional or generalised lymphadenopathy. They can sometimes be difficult to diagnose due to histological confusion between reactive and neoplastic nodes. While their disease is often inherently less chemo-responsive (lower tumour growth/mitotic activity), their tumour is much slower to progress and can often be monitored closely for a long period with no treatment or treated with much less aggressive chemotherapy protocols, such as chlorambucil and prednisolone alone. Discussion of these cases with a clinical oncologist is recommended prior to treatment.
Palliative care only
Dogs may be treated with prednisolone alone and some dogs will respond for a period of three months or so. It is extremely important the owner realises this therapy will make the tumour drug-resistant and deciding at a later point they would like to proceed with chemotherapy is not ideal and likely to seriously affect the dog’s outcome.
Other treatments on the horizon
Rituximab (a CD20 monoclonal antibody) is a standard treatment for humans with large, diffuse B-cell lymphoma (similar to most canine cases), which has revolutionised therapy for people. Unfortunately, despite the fact canine malignant lymphocytes express CD20, rituximab seems to be ineffective. There is, however, a new canine anti-CD20 molecule being trialled with promising provisional results and excellent toxicity profile. Clinical trials of an anti-CD52 molecule for the treatment of T-cell lymphoma are also under way.
Some vaccine trials are in progress in the US and UK, including a DNA vaccine encoding CD20 molecule and also a heat shock protein adjuvant autologous tumour vaccine for dogs with B-cell lymphoma. Provisionally, evidence suggests they can improve outcome in these patients when given in addition to traditional chemotherapy.
Conclusion
For most dogs with lymphoma, the presentation is classical and the diagnosis is very straightforward. Most dogs respond to therapy, at least initially, and the median survival is around a year or so with appropriate therapy (but there is wide variation), and have a very good quality of life.
Despite the vast amount of research into various additional treatments and rescue protocols, the “12-month brick wall” in terms of survival is difficult to breach. Exciting new treatments are on the horizon and are likely to be available for clinical use in the near future.
- Please note some drugs in this article are used under the cascade.
